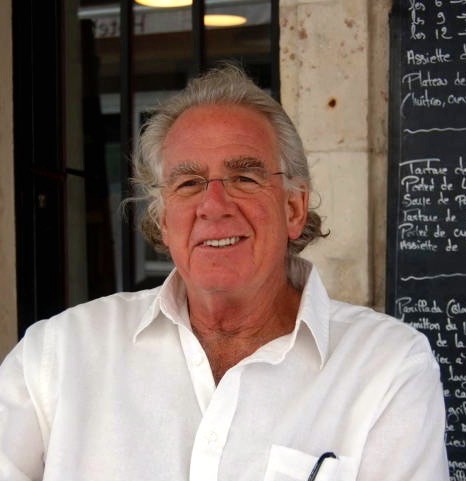
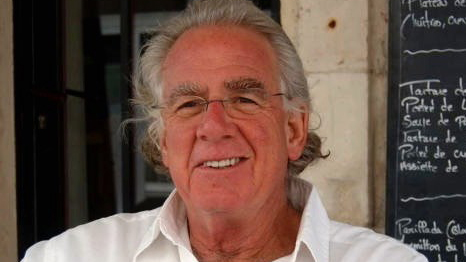
People will often make wild claims about the medical efficacy of cannabis that are, unfortunately, backed by little science. I once heard a speaker at a festival passionately proclaim: “We know THC kills cancer. We know it!” To my knowledge, the woman wasn’t a dedicated researcher conducting clinical trials. She might have been referencing the 2009 study published in the Journal of Clinical Investigation that found that THC might shrink or induce the death of human brain cancer cells. But the study was conducted on mice, meaning “we” don’t know how it will affect people.Which makes me appreciate a film like The Medicine in Marijuana. While it clearly supports medical cannabis, it doesn’t mince words about our need for more research. I spoke with Dr. Ben Daitz, co-writer, -director and -producer of the engaging documentary last week. Dr. Daitz is a professor of Family and Community Medicine and an attending physician at the Pain Consultation and Treatment Center and the Project ECHO pain and headache clinic at UNM.Weekly Alibi: I liked how your film touched on the endocannabinoid system. That’s something that can be confusing to people. Can you explain it briefly?Dr. Daitz: Well I think the film does a reasonably good job of doing that. It really does define why cannabis has the effect that it does—the fact that all humans and all animals, really—down to sponges—have a similar kind of system: the endocannabinoid system. And it’s our own internal cannabinoids, basically. There are receptors that bind with the THC and CBD that is found in the plant, and those receptors that we have are in all parts of our bodies. They’re in our brain—that’s how we can appreciate the fact that THC has an activating effect—it makes you high. But these receptors are also found in our digestive system, in our lungs—in just about every organ in our bodies, in all the tissues. And that accounts, for the most part, why combinations of THC and CBD can help with pain, sleep and appetite.It’s complex biochemistry, but the major ingredients have been figured out. The thing we still don’t know is … cannabis has a bunch of molecules. It’s not just THC and CBD. There are terpenes and other cannabinoids. That’s what we don’t know. We need to do the research. We need to do a lot more than we’re doing right now—particularly in this country.What are the things keeping us from researching it now, other than the Controlled Substances Act?Well that’s the main thing, because it’s very difficult to get a license to do clinical research because of the Controlled Substances Act—because it’s a Schedule I—and it’s a complex plant. For example, people are doing increasing research on LSD and psilocybin. When you look at those, they’re single molecules, but cannabis has multiple molecules. It’s a complex plant, and it’s harder to study—it’s harder to understand. But it’s mostly the rules and the regulations propagated by the federal government in response to Harry Anslinger and others.We’d like to do more research at the School of Medicine, and we are doing qualitative research. We’re trying to look at the interactions between what budtenders tell patients and what patients ask for. That kind of stuff you can do—communication between doctors and patients. Often times we don’t know what our patients are taking. Often times, our patients don’t know what they’re taking. If a patient tells me cannabis helps with their pain, I’ll say, “Well what are you taking?” and they’ll answer, “Well, a little Purple Haze or a little …” Often folks won’t know the concentrations of the cannabinoids, and in order to get more specific about how we educate folks, we need to know about what works for what [condition] and how to measure dosages. That’s the kind of research we need to be doing.New Mexico has a long history of having a medical cannabis program, and yet it’s been very difficult to do research with the data that is stored in the Department of Health’s coffers. The DOH has information on the numbers of people and the conditions, which is obviously reported on in the paper, but we also have good information on demographics. We have information on age and sex and conditions, and we could be scrubbing all that relevant identifying information. We could be doing great research as to what’s helping and what’s not. There’s a trove of information that—particularly because of the past administration—no one has been able to access. It would be wonderful if the School of Medicine and the Department of Health could cooperate and at least start looking at the information that we already have—that the DOH has access to.Do you see any room for improvement in the state’s current medical cannabis program?All the dispensaries have different strains. It’s very complicated, I suspect, for patients trying to make their way through the system. Pharmacists are out of the loop completely. Other states are looking at the education of folks that work in the industry. I think knowing the elements of the endocannabinoid system is important. I think having some basic understanding of what the path of physiology is with these various conditions. That’s potentially a problem we need to start looking at, particularly when it comes to medical cannabis. If you’re trying to make recommendations for a particular condition … we ought to have some method of assessing how much people know and how effective they are at educating their clients.
The Medicine in Marijuana, narrated by Dave Marash, host of the nightly radio program, Here and There, is premiering on New Mexico PBS channel 5 this Friday, Feb. 1, at 8:30pm. The director's cut, which is nearly 10 minutes longer, is available for rent at tijerasfilms.org.